Overview of Microvascular Decompression
Microvascular decompression (MVD) is a surgical procedure designed to treat trigeminal neuralgia, hemifacial spasm, glossopharyngeal neuralgia, and other neurovascular compression syndromes. These conditions are often the result of abnormal compression of a cranial nerve.
Trigeminal neuralgia is the one of the worst pain conditions around. It is often mistakenly diagnosed as a tooth problem as it usually first appears in the lower branches of the trigeminal nerve. Unfortunately, many patients have taken this misdiagnosis and undergone unnecessary, sometimes irreversible, dental procedures.
The condition’s characteristics tend to be episodic, unilateral, shock-like, severe, stabbing, and lancinating.
For the patient, there can be severe pain, suffering, and facial twitching. Chewing, tactile pressure, brushing, shaving, and something as harmless as a breeze of air can exacerbate symptoms.
Women are twice as likely to suffer trigeminal neuralgia as men. Peak ages are in individuals between 50 and 60 years of age. You may get a prescription for a drug like carbamazepine to provide pain relief. However, 10 percent of patients may not respond to drug treatments.
A surgical procedure, MVD, has the potential to offer long-term relief. It minimizes the possibility of postoperative side effects, including numbness. Besides MVD, another option for treating trigeminal neuralgia is Gamma Knife radiosurgery (GKRS). Gamma Knife is a radiation therapy for treating abnormalities in the brain. It is not surgery in the conventional sense as it doesn’t involve an incision. Gamma Knife is often an option for patients who may not quality for procedures like MVD or prefer a non-invasive approach.
Who Should Get MVD
Pending a definitive prognosis, you may be a candidate for microvascular decompression for trigeminal neuralgia under the following conditions.
- You suffer facial pain in the ophthalmic, maxillary and/or mandibular region of your face; any of the three trigeminal areas.
- Your trigeminal neuralgia is not being well-managed with medication alone.
- You want little to no facial numbness that’s associated with other treatments. This includes percutaneous rhizotomy procedures that use either radiofrequency rhizotomy, percutaneous stereotactic rhizotomy, or glycerol injection rhizotomy options.
- You experience recurrence of facial pain after a prior radiological or percutaneous operation.
There are also circumstances where patients may not be eligible for brain procedures that use general anesthesia. This also applies to patients whose ill health is at risk by the surgery.
What You Can Expect – MVD Surgery
Here is a general outline of what to expect from microvascular decompression surgery.
Before Surgery
IMPORTANT – You must always follow the instructions of your MVD surgery team precisely. The comments included here are simply generic and are not meant to be used to modify or supercede any instructions provided by your brain surgeon.
To start, you will review and sign the necessary consent forms and paperwork. These documents are meant to confirm and inform you and your surgeon about your medical history and certain understandings. There may be pre-surgical tests several days before surgery.
Your primary care physician will talk with you about any dietary concerns and what medications you need to stop taking. She will make sure you’re cleared for treatment of trigeminal neuralgia. You will stop taking any non-steroidal anti-inflammatories (naproxen, ibuprofen, etc.) and blood thinners (aspirin, Plavix, Coumadin, etc.) beforehand. You are also advised to stop ingesting alcohol and nicotine a week before and two weeks after the surgery. Otherwise, you increase the risk of bleeding and healing properly.
You shouldn’t drink or eat after midnight before the surgery unless your medical team advising otherwise. If allowed medicines, you will take them with a small sip of water.
During Surgery
After processing for admittance, you will follow five steps to a procedure that generally takes two to three hours.
Preparing the Patient
The anesthesia team will administer general anesthesia. After falling asleep, the surgical team will roll you on your side, placing your head on a skull fixation device. This holds your head still. Antiseptic is applied behind your ear. They may be shaving in the area where the skin incision goes. Also, a team of intra-operative neurophysiologists (a technician and neurologist) connect small recording and stimulating wires to you. These monitor important brain and brainstem functions throughout the entire operation in order to inform the surgical team about the health of your brain in real-time.
Craniectomy
Your brain surgeon will create a short skin incision behind your ear. The surgeon will fold and lift skin and muscle as needed. Now, the surgeon will create a one-inch opening in the occipital bone. With the removal of the bone, the dura is exposed, the protective covering of the brain. Opening that layer with surgical scissors, the dura gets folded back to expose the brain.
Exposing the Nerve
The surface of the cerebellum is protected and relaxed. Next, the surgeon carefully exposes and examines the trigeminal nerve to identify any offending blood vessel. The offending vessel and trigeminal nerve is often protected by thin connective tissue called arachnoid. A small knife and micro scissors are applied to free the tissue and create the necessary space between the vessel and nerve.
Insert a Sponge
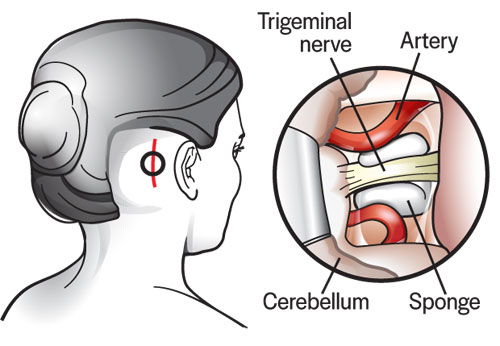
A portion of Teflon sponge is cut to an appropriate size. Now, it’s inserted between the offending vessel and the symptomatic trigeminal nerve. A vein may be adherent to compressing the trigeminal nerve. If so, the vein is cauterize and moved away.
Closing
After the final Teflon sponge is placed and no vessels are in contact with the trigeminal nerve, the surgeon inspects the entire operative field. The dura is sutured closed to form a water-tight closure. Often, a spray on sealant and/or dural patches are used to protect and seal the region.
The bone opening is small, so it’s not replaced with your own bone. Instead, a small titanium plate is placed over the opening and synthetic bone is used for a cosmetic and smooth closure. The muscle is brought back together and the fascia and skin are sutured closed in a layered fashion. Finally, a dressing is placed over the incision.
After Surgery
After monitoring you overnight, you’ll stay until your activity levels are satisfactory. Usually one to two days. After discharge, you’ll receive a series of restrictions and possible prescriptions. It will be important to follow these instructions carefully for two weeks or until a follow-up to ensure long-term health after a microvascular decompression.
Restrictions
Restrictions during the first few weeks after MVD may include:
- Lifting nothing heavier than five pounds.
- No housework, sex, yard work or other strenuous activity.
- No alcohol.
- No nicotine products, including vaping.
- No driving or air travel.
Aftercare
Aftercare may include:
- Gentle washing with mild baby shampoo. Pat drying.
- No submerging in a tub, pool or bath for 2 weeks after surgery.
- No lotion or ointments, including hair-coloring products for 2 weeks after surgery.
Possible Side Effects of Microvascular Decompression
Side effects and complications after microvascular decompression surgery are rare. However, the possibility of a complication is not zero. There may be infection, bleeding, pain recurrence and blood clots in general.
It is important to keep your doctor abreast of your condition after surgery. Any fevers, signs of incision infection, weakness, severe headaches, fluid leaking, swelling, or other issues after the procedure should be reported promptly to ensure safe aftercare following your microvascular decompression.